Induced Pluripotent Stem Cells: Good news on regenerative medicine
The field of regenerative medicine is concerned with healing the diseased and damaged human body. A new method to make pluripotent stem cells discovered by Dr. Yamanaka in 2006, called cellular reprogramming, has enabled Induced Pluripotent Stem Cells (iPSC) to be made from skin cells. A UAB research lead by Michael Edel (PhD) from the Anatomy and Embryology Unity has improved the method of cell reprogramming by substitution of the c-Myc gene (an oncogene) for Cyclin D1. This may pave the way for future clinical applications.
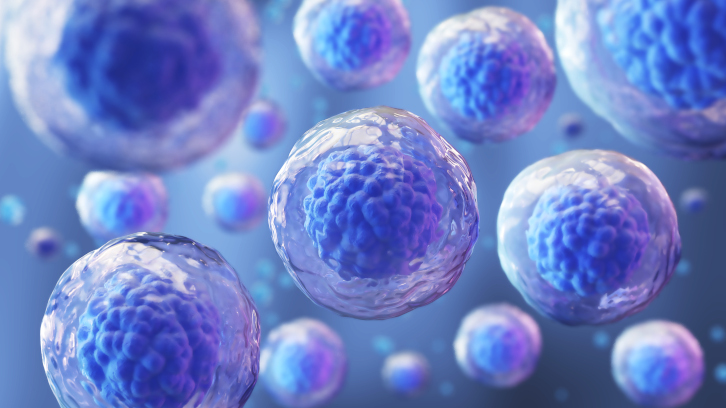
There has been an explosion of research into new technologies surrounding the field of regenerative medicine to advance our ability to heal the aging and damaged human body. At the frontline of the new technology are cell reprogramming methods giving rise to induced pluripotent stem cells (called iPSC) that won the Nobel prize in Medicine for Dr. Yamanaka in 2012. This method opened up a new way to study and treat human disease. The method included using genes Oct3/4, Sox2, Klf4 and c-Myc (a cancer gene) to wind back the clock of the skin cell to form a pluripotent stem cell. There are new regenerative chemicals such as ALK5 inhibitors or mTOR pathway regulators, and neuron survival enhances such as modified curcumin in combination with bioengineered scaffolds and mixed with other adult stem cell types, gene editing methods, all to enhance our ability to regenerate damaged human tissues.
The mission of the laboratory led by Michael Edel (PhD) at the Unit Anatomy and Embryology laboratory based at the UAB, is to perform basic and applied research for iPSC derived cells. The group uses models of human disease to understand how iPSC derived cells such as neurons, corneal eye stem cells on a bioengineered patch or lung stem cells can be used in the clinic for transplantation in patients that otherwise cannot be treated for their damaged or aged tissue.
The research focuses on how to improve the method by Dr. Yamanaka by replacing the cancer gene c-MYC with Cyclin D1 to reprogram skin cells to pluripotent stem cell to improve genetic stability and reduce threat of cancer (1), and to make iPSC cells safer to use in people (1-3). Cyclin D1 just gives a push to the cell growth and proliferation without the effects of the dangerous cancer-causing c-Myc (1). The research is a collaboration with European leaders in genetic stability and cancer here in Spain: Dr. Maria Blasco (CNIO, Twitter: @ADSP_mablasco and @cniostopcancer) and Dr. Manel Esteller (Institute Carreras, Twitter: @manelesteller and @carrerasijc).
Figure 1: A number of barriers need to be addressed to make a skin cell into a pluripotent stem cell (iPSC) that includes, (i) cell size/shape, (ii) increase cell proliferation and (iii) re-set the epigenetic landscape of all the genes in the cell and takes 1-3 month to complete the process. Once iPSC are made any cell of the human body can be made such as neuron stem cells, limbal eye stem cells and lung stem cells to study human disease and in the future for transplantation in people to regenerate aged or damaged tissues.
The use of iPSC to treat human disease and aging has some advantages and disadvantages. Firstly, iPSC reduces the need for using animals in research by screening first with cells in vitro as a model. It also removes ethical issues of embryo destruction to derive pluripotent stem cells, so embryos are not needed anymore. Moreover, immune rejection may be reduced because the cells come from the same person, but still, it may very well be an immune response because of the demanding changes made to the cell to become an iPSC. Regarding the disadvantages, little is known if iPSC derived cells are functional in humans. There have been very few clinical studies in humans, so we still don’t know how they work. Also, they may be dangerous because they are made in the laboratory calling for basic research to improve the method and the cells to reduce the risk of use of these cells once transplanted in humans to treat disease in the future.
Figure 2: Cyclin D1 made improved genetic stability of iPSC.
Will iPSC stem cell Technology ever be safe to use in people? With very little clinical experience with transplanting iPSC derived stem cells such as neurons, cornea eye stem cells or lung stem cells in humans, it is hard to know whether they are safe or very functional. Everything must be done to ensure the cells are safe before using them. The future is likely to bring many more clinical trials involving hiPSC in conditions supported by improved understanding of hiPSC epigenetics and improved tests for cells bearing oncogenic changes (3).
How can this technology be applied? When it comes to Spinal cord injury, iPSC derived neural stem cells have been tested in a model of spinal cord injury (4). The work shows that combining neural stem cells with small chemicals can regenerate neural tissue. With bioengineered scaffolds as well, it can help transplanted neurons to survive that could pave the way for future studies to help return function to people with spinal cord injuries. This research is done in collaboration with Dr. Victoria Moreno (@lab_moreno in Twitter) at the CIPF in Valencia (@cipfvalencia in Instagram and @cipfciencia in Twitter). As for the lung stem cells to treat lung damage, in collaboration with Dr. Ana Belen Alvarez Palomo (Twitter: @belenalpa) from the Banc de Sang i Teixits (BST) Barcelona, demonstrated that iPSC derived lung stem cells can help regenerate damaged fibrotic lungs and that further research is needed to bring that to a clinical testing ready stage (5). For damaged lungs from COVID-19 or other pulmonary viruses, this could be a future option for treatment. As for the cornea eye stem cells, in collaboration with Professor Rafael Barraquer from the Centro Ophthalmology Barraquer (COB. Twitter: @centrobarraquer), Dr. Gemma Julio, Justin D'Antin, Dr. Ricardo Casaroli-Marano and Dr. Ana Belen Alvarez Palomo (Twitter: @belenalpa) (BST), they published together a future road map and review on using iPSC derived limbal stem cells to treat damage to cornea surface of the eye (6) where they concluded that this was a very promising approach at an advanced stage for testing in human clinical trials.
In conclusion, the research by Dr. Michael Edel has improved the cell reprogramming method to generate better genetically stable cells with reduced threat of cancer (1), which addresses one of the main challenges of iPSC for applications to treat human disease. His investigation looks forward to developing the field of iPSC in regenerative medicine to bring it to a point ready for clinical trials to address another major challenge: are iPSC - derived cells functional in humans (2-3)? iPSC -derived cells such as cornea eye stem cells or lung stem cells hold great promise to offer another option for treatment and for patients suffering from debilitating disease (4-6).
Faculty of Medicine
Unit of Anatomy and Embryology
Universitat Autònoma de Barcelona (UAB)
References
1. New improved method to make iPSC for clinical use:
A synthetic mRNA cell reprogramming method using CYCLIN D1 promotes DNA repair, generating improved genetically stable human induced pluripotent stem cells. Alvarez-Palomo AB, Requena-Osete J, Delgado-Morales R, Moreno-Manzano V, Grau-Bove C, Tejera AM, Otero MJ, Barrot C, Santos-Barriopedro I, Vaquero A, Mezquita-Pla J, Moran S, Naya CH, Garcia-Martínez I, Pérez FV, Blasco MA, Esteller M, Edel MJ. Stem Cells. 2021 Jul;39(7):866-881. doi: 10.1002/stem.3358. Epub 2021 Mar 3.PMID: 33621399
2. Stem cells and the immune System:
EDEL, MJ et al, Global Proteomic and Methylome Analysis in Human Induced Pluripotent Stem Cells Reveals Overexpression of a Human TLR3 Affecting Proper Innate Immune Response Signaling. Stem Cells. 2019 Apr;37(4):476-488.
3. Lets talk! Is iPSC safe to use in people?
iPS-Cell Technology and the Problem of Genetic Instability-Can It Ever Be Safe for Clinical Use? Attwood SW, Edel MJ. J Clin Med. 2019 Feb 28;8(3):288. doi: 10.3390/jcm8030288.PMID: 30823421
4. Using iPSC derived neurons to treat spinal injuries:
A Hyaluronic Acid Demilune Scaffold and Polypyrrole-Coated Fibers Carrying Embedded Human Neural Precursor Cells and Curcumin for Surface Capping of Spinal Cord Injuries. Elkhenany H, Bonilla P, Giraldo E, Alastrue Agudo A, Edel MJ, Vicent MJ, Roca FG, Ramos CM, Doblado LR, Pradas MM, Manzano VM. Biomedicines. 2021 Dec 16;9(12):1928. doi: 10.3390/biomedicines9121928.PMID: 34944744
5. Using iPSC derived lung stem cells to treat lung injury:
Induced pluripotent stem cell-derived lung alveolar epithelial type II cells reduce damage in bleomycin-induced lung fibrosis. Alvarez-Palomo B, Sanchez-Lopez LI, Moodley Y, Edel MJ, Serrano-Mollar A. Stem Cell Res Ther. 2020 Jun 3;11(1):213. doi: 10.1186/s13287-020-01726-3.PMID: 32493487
6. Using iPSC derived lung stem cells to treat eye injury:
Potential Role of Induced Pluripotent Stem Cells (IPSCs) for Cell-Based Therapy of the Ocular Surface. Casaroli-Marano RP, Nieto-Nicolau N, Martínez-Conesa EM, Edel M, B Álvarez-Palomo A. J Clin Med. 2015 Feb 12;4(2):318-42. doi: 10.3390/jcm4020318.PMID: 26239129